Teaching topics from the New England Journal of Medicine - Vol. 357, No. 22, November 29, 2007
NEJM Clinical Pearls
Dengue fever and yellow fever are important human viral diseases caused by single-stranded RNA viruses transmitted by insects. Although nearly half the world's population is at risk for infection of dengue fever, and as many as 100 million cases of infection occur annually, there are no antiviral drugs to treat dengue fever and no vaccines to prevent it. Conversely, yellow fever is now largely controlled by vaccination, but many regions are susceptible to a reemergence if the disease is introduced by travelers, and substantial, recent problems with vaccine safety may change vaccination policy.
Dengue Fever and Dengue Hemorrhagic Fever
In its classic form, dengue is an acute illness, characterized by fever, headache, muscle and joint pain, and rash. Immunity against a specific serotype is lifelong, but previous infection with one serotype is a risk factor for a more severe form of dengue — dengue hemorrhagic fever — upon subsequent infection with another serotype. Dengue hemorrhagic fever is characterized by the capillary-leak syndrome, thrombocytopenia, hemorrhage, hypotension, and shock. Approximately 500,000 cases of dengue hemorrhagic fever occur annually, with a case fatality rate ranging from 1 to 3% to as high as 10 to 20%, depending on the available fluid management and intensive care.
Dengue and Yellow Fever Mosquitoes
Dengue and yellow fever are endemic to and epidemic in tropical regions with the principal vector being Aedes aegypti mosquitoes. Infected humans have high blood levels of virus and can therefore infect vector mosquitoes. After an incubation period of about 10 days, during which the virus replicates in a person's salivary-gland tissues, blood-feeding aedes mosquitoes can become infected and transmit the virus to another person. A. aegypti mosquitoes are prevalent in the southern United States, which is therefore receptive to the introduction and spread of both dengue and yellow fever.
Q: What recent problems have occurred with the yellow fever vaccine?
A: Viscerotropic disease, a new syndrome, has been associated with the yellow fever vaccine, an extensive infection of vital organs by a 17D virus that is indistinguishable from wild-type yellow fever disease and has a 60% case fatality rate. Genetic factors of the host (possibly in genes involved in interferon responses) and acquired factors (advanced age and thymectomy) appear to underlie susceptibility to this condition. The overall incidence is about 1 case for every 200,000 to 400,000 vaccinations, but among persons over 60 years of age, the incidence is as high as 1 for every 50,000 vaccinations — which makes 17D one of the least safe vaccines in use.
2007年11月29日 星期四
Radiation Exposure
Teaching topics from the New England Journal of Medicine - Vol. 357, No. 22, November 29, 2007
Abdominal CT versus X-Ray
Organ doses of radiation from CT scanning are considerably larger than those from corresponding conventional radiography. A conventional anterior-posterior abdominal x-ray examination results in a dose to the stomach of approximately 0.25 mGy, which is at least 50 times smaller than the corresponding stomach dose from an abdominal CT scan. A posterior-anterior chest x-ray would result in a radiation dose to the lungs of 0.01 mGy and a lateral chest x-ray, of a radiation dose of 0.15 mGy to the lungs.

Morning Report Questions
Q: Why are more children undergoing diagnostic testing with CT scanning?
A: The major growth area in CT use for children has been for the presurgical diagnosis of appendicitis, for which CT appears to be both accurate and cost-effective — though usually no more so than ultrasonography. A considerable literature questions the use of CT, particularly as a primary diagnostic tool for acute appendicitis in children. A poll of pediatric radiologists (Slovis, Pediatr Radiol, 2002) suggested that perhaps one third of all CT studies could be replaced by alternative approaches or not performed at all.
Q: What is a gray (Gy) — the unit used to describe the radiation dose delivered by a CT scan?
A: Various measures are used to describe the radiation delivered by CT scanning, the most relevant being absorbed dose, effective dose, and CT dose index. The absorbed dose is the energy absorbed per unit of mass and is measured in grays (Gy). One gray equals 1 joule of radiation energy absorbed per kilogram.
Abdominal CT versus X-Ray
Organ doses of radiation from CT scanning are considerably larger than those from corresponding conventional radiography. A conventional anterior-posterior abdominal x-ray examination results in a dose to the stomach of approximately 0.25 mGy, which is at least 50 times smaller than the corresponding stomach dose from an abdominal CT scan. A posterior-anterior chest x-ray would result in a radiation dose to the lungs of 0.01 mGy and a lateral chest x-ray, of a radiation dose of 0.15 mGy to the lungs.

Morning Report Questions
Q: Why are more children undergoing diagnostic testing with CT scanning?
A: The major growth area in CT use for children has been for the presurgical diagnosis of appendicitis, for which CT appears to be both accurate and cost-effective — though usually no more so than ultrasonography. A considerable literature questions the use of CT, particularly as a primary diagnostic tool for acute appendicitis in children. A poll of pediatric radiologists (Slovis, Pediatr Radiol, 2002) suggested that perhaps one third of all CT studies could be replaced by alternative approaches or not performed at all.
Q: What is a gray (Gy) — the unit used to describe the radiation dose delivered by a CT scan?
A: Various measures are used to describe the radiation delivered by CT scanning, the most relevant being absorbed dose, effective dose, and CT dose index. The absorbed dose is the energy absorbed per unit of mass and is measured in grays (Gy). One gray equals 1 joule of radiation energy absorbed per kilogram.
2007年11月21日 星期三
Loffler's endocarditis
NEJM Clinical Pearls
Morning Report Questions
Q: What is Loffler's endocarditis?
A: Loffler's endocarditis is a restrictive cardiomyopathy due to endomyocardial disease with mural thrombi (so-called thrombotic endocarditis) and is secondary to eosinophilia from many causes. Peripheral eosinophilia is almost always present in Loffler's endocarditis, usually present in acute necrotizing eosinophilic myocarditis, sometimes present in hypersensitivity myocarditis, and rarely present in endomyocardial fibrosis (a restrictive cardiomyopathy affecting persons in tropical climates).
Q: What is a known side effect of the medication modafinil used for treatment of fatigue in patients with multiple sclerosis?
A: Modafinil can cause multiorgan hypersensitivity reactions. The Food and Drug Administration now requires a package insert for modafinil that includes this warning. Drugs that have been associated specifically with hypersensitivity myocarditis include antibiotics (sulfonamides, beta-lactams, tetracyclines, aminoglycosides, and others), cardiac medications (methyldopa, dobutamine, thiazides, and furosemide), antiepileptics (phenytoin, carbamazepine), psychotropics, antimycobacterials (streptomycin), and nonsteroidal antiinflammatory drugs.
Acute Eosinophilic Myocarditis
Acute eosinophilic myocarditis (also known as hypersensitivity myocarditis) is caused by a drug hypersensitivity reaction and is characterized by fever, rash, peripheral eosinophilia, and elevated biomarkers of necrosis. ECG occasionally shows ST-segment elevation. Echocardiography reveals mild systolic dysfunction, increased wall thickness due to edema, and occasionally a pericardial effusion. Heart failure is typically mild, and patients die of arrhythmias, rather than pump dysfunction.
Autoimmune Myocarditis and Viral Myocarditis
Autoimmune myocarditis can occur in patients with autoimmune disorders such as systemic lupus erythematosus and polymyositis. Both can cause pericarditis and myocarditis, but the myocarditis tends to be mild. Viral myocarditis is often preceded by a viral syndrome, although this finding is neither sensitive nor specific. Presentations range from slow development of heart failure to rapid development of cardiogenic shock. The ECG often shows nonspecific ST-segment and T-wave abnormalities; echocardiographic findings range from a nondilated left ventricle seen in the acute phase to a spherical, dilated left ventricle in the chronic phase.
Morning Report Questions
Q: What is Loffler's endocarditis?
A: Loffler's endocarditis is a restrictive cardiomyopathy due to endomyocardial disease with mural thrombi (so-called thrombotic endocarditis) and is secondary to eosinophilia from many causes. Peripheral eosinophilia is almost always present in Loffler's endocarditis, usually present in acute necrotizing eosinophilic myocarditis, sometimes present in hypersensitivity myocarditis, and rarely present in endomyocardial fibrosis (a restrictive cardiomyopathy affecting persons in tropical climates).
Q: What is a known side effect of the medication modafinil used for treatment of fatigue in patients with multiple sclerosis?
A: Modafinil can cause multiorgan hypersensitivity reactions. The Food and Drug Administration now requires a package insert for modafinil that includes this warning. Drugs that have been associated specifically with hypersensitivity myocarditis include antibiotics (sulfonamides, beta-lactams, tetracyclines, aminoglycosides, and others), cardiac medications (methyldopa, dobutamine, thiazides, and furosemide), antiepileptics (phenytoin, carbamazepine), psychotropics, antimycobacterials (streptomycin), and nonsteroidal antiinflammatory drugs.
Acute Eosinophilic Myocarditis
Acute eosinophilic myocarditis (also known as hypersensitivity myocarditis) is caused by a drug hypersensitivity reaction and is characterized by fever, rash, peripheral eosinophilia, and elevated biomarkers of necrosis. ECG occasionally shows ST-segment elevation. Echocardiography reveals mild systolic dysfunction, increased wall thickness due to edema, and occasionally a pericardial effusion. Heart failure is typically mild, and patients die of arrhythmias, rather than pump dysfunction.
Autoimmune Myocarditis and Viral Myocarditis
Autoimmune myocarditis can occur in patients with autoimmune disorders such as systemic lupus erythematosus and polymyositis. Both can cause pericarditis and myocarditis, but the myocarditis tends to be mild. Viral myocarditis is often preceded by a viral syndrome, although this finding is neither sensitive nor specific. Presentations range from slow development of heart failure to rapid development of cardiogenic shock. The ECG often shows nonspecific ST-segment and T-wave abnormalities; echocardiographic findings range from a nondilated left ventricle seen in the acute phase to a spherical, dilated left ventricle in the chronic phase.
2007年11月14日 星期三
Diverticulitis
NEJM Clinical Pearls
Diverticulosis: Low Fiber, Constipation, and NSAIDs
The cause of colonic diverticular disease has not yet been conclusively established. Epidemiologic studies have demonstrated associations between diverticulosis and diets that are low in dietary fiber and high in refined carbohydrates. Other factors that have been associated with an increased risk of diverticular disease include physical inactivity, constipation, obesity, smoking, and treatment with nonsteroidal antiinflammatory drugs.
Diverticulitis Symptoms
The clinical manifestations of acute colonic diverticulitis vary with the extent of the disease process. In classic cases, patients report obstipation and abdominal pain that localizes to the left lower quadrant. An abdominal fullness or perirectal fullness, or “mass effect,” may be apparent. Stool guaiac testing may be trace-positive. A low-grade fever is common, as is leukocytosis. Computed tomography (CT) is recommended as the initial radiologic examination.
Morning Report Questions
Q: What is the recommended treatment for a patient suspected of suffering from acute diverticulitis?
A: The decision to hospitalize a patient for diverticulitis depends on the patient's clinical status. For most patients (i.e., immunocompetent patients who have a mild attack and can tolerate oral intake), outpatient therapy is reasonable. This involves 7 to 10 days of oral broad-spectrum antimicrobial therapy, including coverage against anaerobic microorganisms. A combination of ciprofloxacin and metronidazole is often used, but many other combinations are effective. Hospitalization is indicated if the patient is unable to tolerate oral intake or has pain severe enough to require narcotic analgesia or if symptoms fail to improve despite adequate outpatient therapy. Hospitalized patients are usually made NPO (nothing by mouth) and may be candidates for possible nasogastric tube placement if there is evidence of obstruction or ileus.
Q: Is colonoscopy or sigmoidoscopy recommended during an acute diverticulitis attack?
A: Colonoscopy and sigmoidoscopy are typically avoided when acute diverticulitis is suspected because of the risk of perforation or other exacerbation of the disease process. Expert opinion favors performing these tests when the acute process has resolved, usually after approximately 6 weeks, to rule out the presence of other diseases, such as cancer and inflammatory bowel disease.
Diverticulosis: Low Fiber, Constipation, and NSAIDs
The cause of colonic diverticular disease has not yet been conclusively established. Epidemiologic studies have demonstrated associations between diverticulosis and diets that are low in dietary fiber and high in refined carbohydrates. Other factors that have been associated with an increased risk of diverticular disease include physical inactivity, constipation, obesity, smoking, and treatment with nonsteroidal antiinflammatory drugs.
Diverticulitis Symptoms
The clinical manifestations of acute colonic diverticulitis vary with the extent of the disease process. In classic cases, patients report obstipation and abdominal pain that localizes to the left lower quadrant. An abdominal fullness or perirectal fullness, or “mass effect,” may be apparent. Stool guaiac testing may be trace-positive. A low-grade fever is common, as is leukocytosis. Computed tomography (CT) is recommended as the initial radiologic examination.
Morning Report Questions
Q: What is the recommended treatment for a patient suspected of suffering from acute diverticulitis?
A: The decision to hospitalize a patient for diverticulitis depends on the patient's clinical status. For most patients (i.e., immunocompetent patients who have a mild attack and can tolerate oral intake), outpatient therapy is reasonable. This involves 7 to 10 days of oral broad-spectrum antimicrobial therapy, including coverage against anaerobic microorganisms. A combination of ciprofloxacin and metronidazole is often used, but many other combinations are effective. Hospitalization is indicated if the patient is unable to tolerate oral intake or has pain severe enough to require narcotic analgesia or if symptoms fail to improve despite adequate outpatient therapy. Hospitalized patients are usually made NPO (nothing by mouth) and may be candidates for possible nasogastric tube placement if there is evidence of obstruction or ileus.
Q: Is colonoscopy or sigmoidoscopy recommended during an acute diverticulitis attack?
A: Colonoscopy and sigmoidoscopy are typically avoided when acute diverticulitis is suspected because of the risk of perforation or other exacerbation of the disease process. Expert opinion favors performing these tests when the acute process has resolved, usually after approximately 6 weeks, to rule out the presence of other diseases, such as cancer and inflammatory bowel disease.
2007年11月12日 星期一
2007年11月9日 星期五
應小心使用 EPO
FDA Strengthens Warnings on Erythropoiesis-Stimulating Drugs
The FDA has approved additional boxed warnings and label updates for the erythropoiesis-stimulating agents Aranesp, Epogen, and Procrit.
The new warnings note that when the drugs were dosed to achieve hemoglobin levels over 12 g/dL, they stimulated tumor growth and decreased survival in patients with advanced breast, head and neck, lymphoid, and non-small cell lung cancer. (Higher mortality and tumor progression have not been ruled out at levels under 12 g/dL.)
When used to maintain hemoglobin levels over 12 g/dL in patients with chronic renal failure, the drugs increased the risk for death, stroke, heart attack, and heart failure. In these patients, the FDA recommends aiming for hemoglobin levels between 10 and 12 g/dL.
參考:
http://www.fda.gov/bbs/topics/NEWS/2007/NEW01740.html
The FDA has approved additional boxed warnings and label updates for the erythropoiesis-stimulating agents Aranesp, Epogen, and Procrit.
The new warnings note that when the drugs were dosed to achieve hemoglobin levels over 12 g/dL, they stimulated tumor growth and decreased survival in patients with advanced breast, head and neck, lymphoid, and non-small cell lung cancer. (Higher mortality and tumor progression have not been ruled out at levels under 12 g/dL.)
When used to maintain hemoglobin levels over 12 g/dL in patients with chronic renal failure, the drugs increased the risk for death, stroke, heart attack, and heart failure. In these patients, the FDA recommends aiming for hemoglobin levels between 10 and 12 g/dL.
參考:
http://www.fda.gov/bbs/topics/NEWS/2007/NEW01740.html
2007年11月7日 星期三
Bacterial Meningitis
NEJM Clinical Pearls
Common Organisms in Bacterial Meningitis
The most common bacteria causing meningitis in adults are Streptococcus pneumoniae (about half of cases), Neisseria meningitidis (about one fifth of cases), Listeria monocytogenes (about one tenth of cases), and Haemophilus influenzae (about one tenth of cases). The otitic meningitis in this patient (whose ear infection may have caused bony erosion that led to a cerebrospinal fluid fistula) prompted the clinicians to consider more aggressive organisms such as Staphylococcus aureus, gram-negative organisms, and group A streptococcus. In fact, blood and cerebrospinal cultures became positive for group A streptococcus within a few hours.
Group A Streptococcus Meningitis
Infections with group A streptococcus are a rare cause of bacterial meningitis, accounting for 0.5 to 1.5% of community-acquired cases; the mortality rate (27%) is similar to that for pneumococcal meningitis (30%). Otitis media due to group A streptococcus is associated with high rates of local invasion, including tympanic perforation and mastoiditis, and this form of otitis media is the most important risk factor for group streptococcal meningitis among adult patients. Most patients with group A streptococcal meningitis do not have the clinical features of septic shock associated with invasive streptococcal disease, and the incidence of group A streptococcal meningitis has not increased, despite an increasing incidence of other forms of invasive disease.
Morning Report Question
Q: An important clinical challenge is how to recognize when fluid emanating from the ear or the nose is, in fact, cerebrospinal fluid. How might this be accomplished?
A: Otorrhea and rhinorrhea may be recognized as containing cerebrospinal fluid if the fluid has a relatively low protein level (less than 2 g/L) and should be clinically suspected when a handkerchief or cloth soaked in the fluid does not stiffen when dry. A fluid glucose level of greater than 40 mg per deciliter (2.2 mmol per liter) also suggests that the fluid is cerebrospinal fluid. The most accurate test is a measurement of β2-transferrin, a protein that is found only in cerebrospinal fluid. Of note, cerebrospinal fluid otorrhea may be serosanguineous and mistaken for blood.
Common Organisms in Bacterial Meningitis
The most common bacteria causing meningitis in adults are Streptococcus pneumoniae (about half of cases), Neisseria meningitidis (about one fifth of cases), Listeria monocytogenes (about one tenth of cases), and Haemophilus influenzae (about one tenth of cases). The otitic meningitis in this patient (whose ear infection may have caused bony erosion that led to a cerebrospinal fluid fistula) prompted the clinicians to consider more aggressive organisms such as Staphylococcus aureus, gram-negative organisms, and group A streptococcus. In fact, blood and cerebrospinal cultures became positive for group A streptococcus within a few hours.
Group A Streptococcus Meningitis
Infections with group A streptococcus are a rare cause of bacterial meningitis, accounting for 0.5 to 1.5% of community-acquired cases; the mortality rate (27%) is similar to that for pneumococcal meningitis (30%). Otitis media due to group A streptococcus is associated with high rates of local invasion, including tympanic perforation and mastoiditis, and this form of otitis media is the most important risk factor for group streptococcal meningitis among adult patients. Most patients with group A streptococcal meningitis do not have the clinical features of septic shock associated with invasive streptococcal disease, and the incidence of group A streptococcal meningitis has not increased, despite an increasing incidence of other forms of invasive disease.
Morning Report Question
Q: An important clinical challenge is how to recognize when fluid emanating from the ear or the nose is, in fact, cerebrospinal fluid. How might this be accomplished?
A: Otorrhea and rhinorrhea may be recognized as containing cerebrospinal fluid if the fluid has a relatively low protein level (less than 2 g/L) and should be clinically suspected when a handkerchief or cloth soaked in the fluid does not stiffen when dry. A fluid glucose level of greater than 40 mg per deciliter (2.2 mmol per liter) also suggests that the fluid is cerebrospinal fluid. The most accurate test is a measurement of β2-transferrin, a protein that is found only in cerebrospinal fluid. Of note, cerebrospinal fluid otorrhea may be serosanguineous and mistaken for blood.
2007年11月6日 星期二
Patrick's (or FABER) Test

Patrick's test stresses the hip and sacroiliac joints. A positive test produces back, buttocks, or groin pain. The thigh and knee of the supine patient are flexed, and the external malleolus of the ankle is placed over the patella of the opposite leg. The test is positive if depression of the knee produces pain.
- The Patrick or FABER test is a screening test for pathology of the hip joint or sacrum.
- The test is performed as follows: Place the patient in the supine position. Flex the leg and put the foot of the tested leg on the opposite knee (the motion is that of Flexion, ABduction, External Rotation at the hip). Slowly press down on the superior aspect of the tested knee joint lowering the leg into further abduction
- The test is positive if there is pain at the hip or sacral joint, or if the leg can not lower to the point of being parallel to the opposite leg.
2007年11月5日 星期一
2007年11月4日 星期日
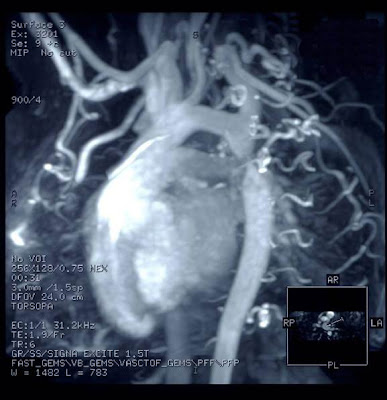
Aortic coarctation
2007年11月2日 星期五
EGDT Can Save Lives
Early Goal-Directed Therapy Can Save Lives (and Money)
EDs and ICUs should work together to implement this treatment for patients with severe sepsis and septic shock.
Although early goal-directed therapy (EGDT) has been shown to improve outcomes in severe sepsis and septic shock, clinical implementation has been slow. Barriers such as cost, emergency department overcrowding, lack of training, and institutional resistance present significant challenges to use of EGDT. To assess the economic consequences of implementing EGDT, researchers conducted a decision analysis of three implementation strategies: ED-centric (all treatment administered in the ED), mobile intensive care unit (ICU) team (ED screens patients and then alerts the ICU team, which provides EGDT), and ICU-centric (EGDT administered in the ICU after ED transfer).
Estimates were derived using data from multiple sources, including the Henry Ford Health System, Medicare, the U.S. Public Health Service, and the American Thoracic Society. Analyses were based on assumptions that an average ED has an annual volume of 29,100 visits and 91 cases of severe sepsis and septic shock. The authors estimated that start-up costs would range from US$13,000 (ICU-centric) to $30,000 (ED-centric) and that additional annual costs would be $100,000.
Compared with usual care, EGDT saved an estimated mean of $8,666 per patient, representing a 22.9% reduction in hospital costs per patient and a yearly savings of nearly $800,000 per hospital. The savings were due primarily to a reduction in length of ICU stay. Although the ICU-centric model was the least costly, it was also the least effective because of time delays. In sensitivity analysis, EGDT remained cost-effective in all three models even when the mortality benefit was reduced by almost half. Cost per quality-adjusted life-year was $7,019 in the ED-centric model, $6,931 in the ICU-team model, and $2,749 in the ICU-centric model.
Comment:
EGDT can save lives and money — even according to a conservative model that was created with bias against EGDT’s cost-effectiveness by assigning substantial start-up costs. In addition, EGDT remained cost-effective in sensitivity analysis that was further biased against it by substantially reducing the mortality benefit. Although EDs have the infrastructure to manage critically ill cases, the authors included in their analyses costs not only for increased staffing, training, and screening but also for upgrading two additional rooms for invasive monitoring. EDs and ICUs should work together to implement EGDT, as it benefits both hospitals and patients.
— Tiffany M. Osborn, MD
Published in Journal Watch Emergency Medicine November 2, 2007
Citation(s):Huang DT et al. Implementation of early goal-directed therapy for severe sepsis and septic shock: A decision analysis. Crit Care Med 2007 Sep; 35:2090.
EDs and ICUs should work together to implement this treatment for patients with severe sepsis and septic shock.
Although early goal-directed therapy (EGDT) has been shown to improve outcomes in severe sepsis and septic shock, clinical implementation has been slow. Barriers such as cost, emergency department overcrowding, lack of training, and institutional resistance present significant challenges to use of EGDT. To assess the economic consequences of implementing EGDT, researchers conducted a decision analysis of three implementation strategies: ED-centric (all treatment administered in the ED), mobile intensive care unit (ICU) team (ED screens patients and then alerts the ICU team, which provides EGDT), and ICU-centric (EGDT administered in the ICU after ED transfer).
Estimates were derived using data from multiple sources, including the Henry Ford Health System, Medicare, the U.S. Public Health Service, and the American Thoracic Society. Analyses were based on assumptions that an average ED has an annual volume of 29,100 visits and 91 cases of severe sepsis and septic shock. The authors estimated that start-up costs would range from US$13,000 (ICU-centric) to $30,000 (ED-centric) and that additional annual costs would be $100,000.
Compared with usual care, EGDT saved an estimated mean of $8,666 per patient, representing a 22.9% reduction in hospital costs per patient and a yearly savings of nearly $800,000 per hospital. The savings were due primarily to a reduction in length of ICU stay. Although the ICU-centric model was the least costly, it was also the least effective because of time delays. In sensitivity analysis, EGDT remained cost-effective in all three models even when the mortality benefit was reduced by almost half. Cost per quality-adjusted life-year was $7,019 in the ED-centric model, $6,931 in the ICU-team model, and $2,749 in the ICU-centric model.
Comment:
EGDT can save lives and money — even according to a conservative model that was created with bias against EGDT’s cost-effectiveness by assigning substantial start-up costs. In addition, EGDT remained cost-effective in sensitivity analysis that was further biased against it by substantially reducing the mortality benefit. Although EDs have the infrastructure to manage critically ill cases, the authors included in their analyses costs not only for increased staffing, training, and screening but also for upgrading two additional rooms for invasive monitoring. EDs and ICUs should work together to implement EGDT, as it benefits both hospitals and patients.
— Tiffany M. Osborn, MD
Published in Journal Watch Emergency Medicine November 2, 2007
Citation(s):Huang DT et al. Implementation of early goal-directed therapy for severe sepsis and septic shock: A decision analysis. Crit Care Med 2007 Sep; 35:2090.
訂閱:
意見 (Atom)