LP Is Not Needed for Young Children with First Simple Febrile Seizure
It is time for the American Academy of Pediatrics to revise its recommendations for LP.
Although first simple febrile seizure (FSFS) usually is not the sole manifestation of bacterial meningitis, the American Academy of Pediatrics (AAP) practice parameter for the diagnostic evaluation of FSFS in children recommends that lumbar puncture (LP) be "strongly considered" for patients younger than 12 months and "considered" for those aged 12 to 18 months (Pediatrics 1996; 97:769). Investigators challenged this recommendation in the era of Haemophilus influenzae type B and pneumococcal conjugate vaccines.
The investigators retrospectively reviewed charts of well-appearing children aged 6 to 18 months who presented within 12 hours after FSFS to a single emergency department in Boston between 1995 and 2006. The primary outcome was the rate of bacterial meningitis. Secondary outcomes were compliance with the AAP practice parameter and temporal trends in the performance of LP. Of 704 patients, 27% were younger than 12 months. Overall, 8% of patients were hospitalized, and 10% had received at least one dose of antibiotics before their ED visit. LP was attempted in 271 cases (38%), and cerebrospinal fluid (CSF) was obtained in 260. Ten cases (3.8%) had CSF pleocytosis (median white cell count, 1 cell/mm3). No CSF culture was positive for a pathogen, and no patients with CSF pleocytosis had positive blood cultures. None of the 704 patients returned to the hospital with bacterial meningitis. During the study period, LP was performed in 70% of patients younger than 12 months and in 25% of those aged 12 to 18 months, with rates decreasing over time in both age groups. The authors recommend changing the wording of the AAP practice parameter to simply state that "meningitis should be considered in the differential diagnosis for any febrile child, and LP should be performed if there are clinical signs or symptoms of concern."
Comment:
Most children with apparent FSFS who turn out to have meningitis also present with altered mental status and other clinical signs of meningitis. Given the low probability of bacterial meningitis in the current era of conjugate vaccines, there is no reason to assume that a febrile child aged 6 to 18 months with FSFS has an appreciable risk for meningitis; therefore, LP is not indicated. These data support a revision of the AAP practice parameter.
—
Jill M. Baren, MD, MBE, FACEP, FAAP
Published in Journal Watch Emergency Medicine February 27, 2009
Citation(s): Kimia AA et al. Utility of lumbar puncture for first simple febrile seizure among children 6 to 18 months of age. Pediatrics 2009 Jan; 123:6.
2009年2月27日 星期五
2009年2月26日 星期四
2009年2月20日 星期五
Fibrinolytic therapy in pulmonary embolism

Patients presenting with pulmonary embolism (PE) have a wide spectrum of clinical severity. Although some patients may present with frank hemodynamic collapse and cardiac arrest, others may present with an asymptomatic PE that is discovered incidentally during workup of another condition. Fibrinolytic therapy is an option in the treatment of patients with PE due to its ability to rapidly dissolve thromboemboli clots. However, the use of fibrinolytics in the treatment of PE is a controversial topic that has left many practicing physicians confused on how to best treat these patients. A rational approach to deciding whether fibrinolytic therapy is indicated is based on an assessment of the benefit that each particular patient will derive from fibrinolytic therapy weighed against that patients risk for major bleeding and intracranial hemorrhage. There is a clear benefit/risk ratio for fibrinolytic therapy in patients with PE who present with cardiac arrest and in those who are hemodynamically unstable from a massive PE. With proper risk assessment, select patients with stable hemodynamics and right ventricular dysfunction may also benefit from fibrinolytic therapy. There is no benefit to fibrinolytic treatment in patients with stable hemodynamics and normal right ventricular function. This article sets out to review the literature on fibrinolytic therapy in the treatment of patients with PE and will propose an evidence based treatment algorithm.
---------
全文 (密碼:2833....):
或
2009年2月19日 星期四
流鼻血...
Epistaxis: Local and Systemic Causes
Local causes contributing to epistaxis include self-induced digital trauma (nose picking), topical nasal drugs including corticosteroids and antihistamines, illicit nasal drug use, dry mucosa, viral or bacterial rhinosinusitis and neoplasms. Systemic conditions associated with epistaxis include genetic disorders such as hemophilia, acquired coagulopathies, anticoagulant medication, or hematologic cancers. Low-dose aspirin appears to increase the risk of epistaxis slightly. Alternative therapies, such as ingestion of garlic, ginkgo, or ginseng may also contribute to mild systemic coagulopathies and epistaxis.
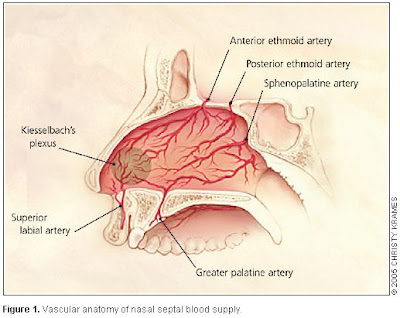
Anterior versus Posterior Bleeding
More than 90% of episodes of epistaxis occur along the anterior nasal septum at a site called Kiesselbach's area. This area receives blood from the terminal branches of the sphenopalatine, ethmoidal, and superior labial arteries. Anterior epistaxis is most often self-limited and does not require medical attention. Pinching the anterior aspect of the nose (not the nasal bones) provides tamponade for the anterior septal vessels and use of topical vasoconstrictors and anesthetics (combination of lidocaine or ponticaine with phenylephrine or oxymetazoline spray) and topical moisturizing ointments can be of value. The patient should relax, tip the head forward or backward, and avoid swallowing or aspirating any blood that may be draining down the posterior pharynx. Packing the nose with absorbable hemostatic materials or chemical (silver nitrate) or electrical cautery is sometimes necessary. Approximately 10% of nosebleeds occur posteriorly, along the nasal septum or lateral nasal wall.
What is the most common type of epistaxis among the elderly, anterior or posterior?
A: Posterior nose bleeds are more common in older patients (mean age 64 years). Anterior nose bleeds, at a site called Kiesselbach's area is the more common type of epistaxis among children. The prevalence of epistaxis in general is increased for children less than 10 years of age and then rises again after the age of 35 years.
How common are coagulopathies in patients hospitalized for epistaxis?
A: Forty-five percent of patients hospitalized for epistaxis have systemic disorders with the potential to contribute to nosebleeds, including genetic disorders such as hemophilia and acquired coagulopathies due to liver or renal disease, use of anticoagulant medication, or hematologic cancers.
---
Source:
New England Journal of Medicine - Vol. 360, No. 8, February 19, 2009
More reading:
http://www.aafp.org/afp/20050115/305.pdf
2009年2月18日 星期三
Left main及triple vessle之CAD:CABG比PCI好!
Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease
Background
Percutaneous coronary intervention (PCI) involving drug-eluting stents is increasingly used to treat complex coronary artery disease, although coronary-artery bypass grafting (CABG) has been the treatment of choice historically. Our trial compared PCI and CABG for treating patients with previously untreated three-vessel or left main coronary artery disease (or both).
Methods
We randomly assigned 1800 patients with three-vessel or left main coronary artery disease to undergo CABG or PCI (in a 1:1 ratio). For all these patients, the local cardiac surgeon and interventional cardiologist determined that equivalent anatomical revascularization could be achieved with either treatment. A noninferiority comparison of the two groups was performed for the primary end point — a major adverse cardiac or cerebrovascular event (i.e., death from any cause, stroke, myocardial infarction, or repeat revascularization) during the 12-month period after randomization. Patients for whom only one of the two treatment options would be beneficial, because of anatomical features or clinical conditions, were entered into a parallel, nested CABG or PCI registry.
Results
Most of the preoperative characteristics were similar in the two groups. Rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the PCI group (17.8%, vs. 12.4% for CABG; P=0.002), in large part because of an increased rate of repeat revascularization (13.5% vs. 5.9%, P<0.001); as a result, the criterion for noninferiority was not met. At 12 months, the rates of death and myocardial infarction were similar between the two groups; stroke was significantly more likely to occur with CABG (2.2%, vs. 0.6% with PCI; P=0.003).
Conclusions
CABG remains the standard of care for patients with three-vessel or left main coronary artery disease, since the use of CABG, as compared with PCI, resulted in lower rates of the combined end point of major adverse cardiac or cerebrovascular events at 1 year. (ClinicalTrials.gov number, NCT00114972 [ClinicalTrials.gov] .)
----
Published at www.nejm.org February 18, 2009 (10.1056/NEJMoa0804626)
http://content.nejm.org/cgi/content/full/NEJMoa0804626
Background
Percutaneous coronary intervention (PCI) involving drug-eluting stents is increasingly used to treat complex coronary artery disease, although coronary-artery bypass grafting (CABG) has been the treatment of choice historically. Our trial compared PCI and CABG for treating patients with previously untreated three-vessel or left main coronary artery disease (or both).
Methods
We randomly assigned 1800 patients with three-vessel or left main coronary artery disease to undergo CABG or PCI (in a 1:1 ratio). For all these patients, the local cardiac surgeon and interventional cardiologist determined that equivalent anatomical revascularization could be achieved with either treatment. A noninferiority comparison of the two groups was performed for the primary end point — a major adverse cardiac or cerebrovascular event (i.e., death from any cause, stroke, myocardial infarction, or repeat revascularization) during the 12-month period after randomization. Patients for whom only one of the two treatment options would be beneficial, because of anatomical features or clinical conditions, were entered into a parallel, nested CABG or PCI registry.
Results
Most of the preoperative characteristics were similar in the two groups. Rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the PCI group (17.8%, vs. 12.4% for CABG; P=0.002), in large part because of an increased rate of repeat revascularization (13.5% vs. 5.9%, P<0.001); as a result, the criterion for noninferiority was not met. At 12 months, the rates of death and myocardial infarction were similar between the two groups; stroke was significantly more likely to occur with CABG (2.2%, vs. 0.6% with PCI; P=0.003).
Conclusions
CABG remains the standard of care for patients with three-vessel or left main coronary artery disease, since the use of CABG, as compared with PCI, resulted in lower rates of the combined end point of major adverse cardiac or cerebrovascular events at 1 year. (ClinicalTrials.gov number, NCT00114972 [ClinicalTrials.gov] .)
----
Published at www.nejm.org February 18, 2009 (10.1056/NEJMoa0804626)
http://content.nejm.org/cgi/content/full/NEJMoa0804626
2009年2月11日 星期三
Lactate clearance 不適用於 trauma??
Prognostic Value of Blood Lactate Levels: Does the Clinical Diagnosis at Admission Matter?
The Journal of Trauma: Injury, Infection, and Critical Care:Volume 66(2)February 2009pp 377-385
Background:
Hyperlactatemia and its reduction after admission in the intensive care unit (ICU) have been related to survival. Because it is unknown whether this equally applies to different groups of critically ill patients, we compared the prognostic value of repeated lactate levels (a) in septic patients versus patients with hemorrhage or other conditions generally associated with low-oxygen transport (LT) (b) in hemodynamically stable versus unstable patients.
Methods:
In this prospective observational two-center study (n = 394 patients), blood lactate levels at admission to the ICU (LacT0) and the reduction of lactate levels from T = 0 to T = 12 hours (ΔLacT0-12) and from T = 12 to T = 24 hours (ΔLacT12-24), were related to in-hospital mortality.
Results:
Reduction of lactate was associated with a lower mortality only in the sepsis group (ΔLacT0-12: hazard ratio [HR] 0.34, p = 0.004 and ΔLacT12-24: HR 0.24, p = 0.003), but not in the LT group (ΔLacT0-12; HR 0.78, p = 0.52 and ΔLacT12-24; HR 1.30, p = 0.61). The prognostic values of LacT0, ΔLacT0-12, and ΔLacT12-24 were similar in hemodynamically stable and unstable patients (p = 0.43).
Conclusions:
Regardless of the hemodynamic status, lactate reduction during the first 24 hours of ICU stay is associated with improved outcome only in septic patients, but not in patients with hemorrhage or other conditions generally associated with low-oxygen transport (LT). We hypothesize that in this particular group a reduction in lactate is not associated with improved outcome due to irreversible damage at ICU admission.
The Journal of Trauma: Injury, Infection, and Critical Care:Volume 66(2)February 2009pp 377-385
Background:
Hyperlactatemia and its reduction after admission in the intensive care unit (ICU) have been related to survival. Because it is unknown whether this equally applies to different groups of critically ill patients, we compared the prognostic value of repeated lactate levels (a) in septic patients versus patients with hemorrhage or other conditions generally associated with low-oxygen transport (LT) (b) in hemodynamically stable versus unstable patients.
Methods:
In this prospective observational two-center study (n = 394 patients), blood lactate levels at admission to the ICU (LacT0) and the reduction of lactate levels from T = 0 to T = 12 hours (ΔLacT0-12) and from T = 12 to T = 24 hours (ΔLacT12-24), were related to in-hospital mortality.
Results:
Reduction of lactate was associated with a lower mortality only in the sepsis group (ΔLacT0-12: hazard ratio [HR] 0.34, p = 0.004 and ΔLacT12-24: HR 0.24, p = 0.003), but not in the LT group (ΔLacT0-12; HR 0.78, p = 0.52 and ΔLacT12-24; HR 1.30, p = 0.61). The prognostic values of LacT0, ΔLacT0-12, and ΔLacT12-24 were similar in hemodynamically stable and unstable patients (p = 0.43).
Conclusions:
Regardless of the hemodynamic status, lactate reduction during the first 24 hours of ICU stay is associated with improved outcome only in septic patients, but not in patients with hemorrhage or other conditions generally associated with low-oxygen transport (LT). We hypothesize that in this particular group a reduction in lactate is not associated with improved outcome due to irreversible damage at ICU admission.
2009年2月6日 星期五
按摩棒走後門 啊…捅破愛妻直腸

X光片中明顯看出情趣按摩棒在婦人體內。(記者徐夏蓮翻攝)
台中市傳出一對30多歲的夫妻一大清早「炒 飯」,還使用情趣按摩棒「走後門」,沒想到發生「棒穿腸出」的傷人憾事,為此,這名少婦付出腹部15公分傷口、直腸破裂需修補的慘痛代價,住院一週才趕在農曆年前出院。
台中醫院急診室主任王史典昨天指出,這對30多歲的夫妻,在早上8點左右掛急診,經X光照射,有根狀似按摩棒的東西卡在婦人直腸附近,直腸外科主任蔡金宏原本想以肛門鏡將棒子拖出來,但找不到著力點,改為剖腹想利用腸子擠壓的方式,讓按摩棒從腸子經肛門出來,但肚子一打開,這根按摩棒已破腸而出了。
為了這根情趣按摩棒,這名婦人直腸近乙狀結腸破洞,醫師花了一個半小時才修補完成,蔡金宏表示,幸好棒子在24小時內取出,傷口也很單純,否則可能因感 染等原因,又出現其他更難收拾的後遺症。
台中醫院急診室主任王史典指出,這對夫婦可能發現棒子跑進去、拿不出來後心急地想取出,才更讓這根長18公分、直徑約4至5公分的按摩棒更長驅直入。
中市性教育講師黃瑞汝則說,如今工作壓力大、失業率高,男的勃起不易、硬度不夠,女的高潮困難者,比比皆是,她肯定夫妻或情侶使用情趣用品「突困」的精神,但建議一定要詳看使用說明書,並注意安全。
台中市傳出一對30多歲的夫妻一大清早「炒 飯」,還使用情趣按摩棒「走後門」,沒想到發生「棒穿腸出」的傷人憾事,為此,這名少婦付出腹部15公分傷口、直腸破裂需修補的慘痛代價,住院一週才趕在農曆年前出院。
台中醫院急診室主任王史典昨天指出,這對30多歲的夫妻,在早上8點左右掛急診,經X光照射,有根狀似按摩棒的東西卡在婦人直腸附近,直腸外科主任蔡金宏原本想以肛門鏡將棒子拖出來,但找不到著力點,改為剖腹想利用腸子擠壓的方式,讓按摩棒從腸子經肛門出來,但肚子一打開,這根按摩棒已破腸而出了。
為了這根情趣按摩棒,這名婦人直腸近乙狀結腸破洞,醫師花了一個半小時才修補完成,蔡金宏表示,幸好棒子在24小時內取出,傷口也很單純,否則可能因感 染等原因,又出現其他更難收拾的後遺症。
台中醫院急診室主任王史典指出,這對夫婦可能發現棒子跑進去、拿不出來後心急地想取出,才更讓這根長18公分、直徑約4至5公分的按摩棒更長驅直入。
中市性教育講師黃瑞汝則說,如今工作壓力大、失業率高,男的勃起不易、硬度不夠,女的高潮困難者,比比皆是,她肯定夫妻或情侶使用情趣用品「突困」的精神,但建議一定要詳看使用說明書,並注意安全。
〔記者徐夏蓮、許國楨/台中報導〕
2009年2月4日 星期三
Chronic Diarrhea
Differential Diagnosis of Chronic Diarrhea
The differential diagnosis of chronic diarrhea (i.e., diarrhea lasting at least 4 to 6 weeks) includes chronic and relapsing gastrointestinal infection, inflammatory bowel disease, microscopic colitis, malabsorption syndromes, medication side effects, endocrine disorders, laxative abuse, colonic neoplasia, and idiopathic (functional) diarrhea, as well as neuroendocrine tumors. Guidelines recommend using the history and the findings on physical examination plus laboratory testing to categorize chronic diarrhea as secretory, osmotic, inflammatory, or fatty; this categorization can narrow the differential diagnosis and guide further testing.
What red-flag signs should not be missed in patients with chronic diarrhea?
A: In patients with chronic diarrhea, so-called alarm or red-flag signs include weight loss, nocturnal symptoms, a family history of colorectal cancer, rectal bleeding, or anemia; any of these signs and symptoms would warrant further evaluation.
In a patient with chronic diarrhea, what features might distinguish an organic versus a functional cause (such as irritable bowel syndrome)?
A: Historical features that suggest an organic as opposed to a functional cause of chronic diarrhea, such as irritable bowel syndrome, include a shorter duration of diarrhea (less than 3 months), nocturnal diarrhea, an abrupt onset of diarrhea, weight loss of more than 11 lb (5.0 kg), and stool weight of more than 400 g per day. Common causes of chronic diarrhea include the irritable bowel syndrome, inflammatory bowel disease, malabsorption syndromes, and chronic infections, particularly in patents who are immunocompromised.
What disorder involving the small bowel is associated with Graves' disease?
A: Celiac disease is common among patients with Graves' disease.
---
New England Journal of Medicine - Vol. 360, No. 6, February 5, 2009
The differential diagnosis of chronic diarrhea (i.e., diarrhea lasting at least 4 to 6 weeks) includes chronic and relapsing gastrointestinal infection, inflammatory bowel disease, microscopic colitis, malabsorption syndromes, medication side effects, endocrine disorders, laxative abuse, colonic neoplasia, and idiopathic (functional) diarrhea, as well as neuroendocrine tumors. Guidelines recommend using the history and the findings on physical examination plus laboratory testing to categorize chronic diarrhea as secretory, osmotic, inflammatory, or fatty; this categorization can narrow the differential diagnosis and guide further testing.
What red-flag signs should not be missed in patients with chronic diarrhea?
A: In patients with chronic diarrhea, so-called alarm or red-flag signs include weight loss, nocturnal symptoms, a family history of colorectal cancer, rectal bleeding, or anemia; any of these signs and symptoms would warrant further evaluation.
In a patient with chronic diarrhea, what features might distinguish an organic versus a functional cause (such as irritable bowel syndrome)?
A: Historical features that suggest an organic as opposed to a functional cause of chronic diarrhea, such as irritable bowel syndrome, include a shorter duration of diarrhea (less than 3 months), nocturnal diarrhea, an abrupt onset of diarrhea, weight loss of more than 11 lb (5.0 kg), and stool weight of more than 400 g per day. Common causes of chronic diarrhea include the irritable bowel syndrome, inflammatory bowel disease, malabsorption syndromes, and chronic infections, particularly in patents who are immunocompromised.
What disorder involving the small bowel is associated with Graves' disease?
A: Celiac disease is common among patients with Graves' disease.
---
New England Journal of Medicine - Vol. 360, No. 6, February 5, 2009
Respiratory Syncytial Virus
Respiratory Syncytial Virus Infection in Children
Among children under the age of 5 years, RSV infection results in approximately 1 of 334 hospitalizations, 1 of 38 visits to an emergency department, and 1 of 13 visits to a primary care office each year in the United States. An estimated 2.1 million children under 5 years of age with RSV infection require medical attention each year. Among these children with RSV-related illnesses, approximately 3% are hospitalized, 25% are treated in emergency departments, and 73% are treated in pediatric practices. Of those seen as outpatients, 61% are between 2 and 5 years of age.
Risk Factors for RSV
In this study by Hall and colleagues, characteristics that were most frequently associated with RSV illness requiring hospitalization included male sex, chronic coexisting medical conditions, lower socioeconomic status, smoke exposure, lack of breast-feeding, and contact with other children. None of these factors independently correlated with illness severity except for young age and prematurity.
What drug is used for RSV prophylaxis in high-risk infants and children?
A: Palivizumab (Synagis) is used as prophylaxis against RSV as a monthly injection in high-risk children. There is no RSV vaccine available.
---
New England Journal of Medicine - Vol. 360, No. 6, February 5, 2009
Hall CB et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med 2009 Feb 5; 360:588.
Among children under the age of 5 years, RSV infection results in approximately 1 of 334 hospitalizations, 1 of 38 visits to an emergency department, and 1 of 13 visits to a primary care office each year in the United States. An estimated 2.1 million children under 5 years of age with RSV infection require medical attention each year. Among these children with RSV-related illnesses, approximately 3% are hospitalized, 25% are treated in emergency departments, and 73% are treated in pediatric practices. Of those seen as outpatients, 61% are between 2 and 5 years of age.
Risk Factors for RSV
In this study by Hall and colleagues, characteristics that were most frequently associated with RSV illness requiring hospitalization included male sex, chronic coexisting medical conditions, lower socioeconomic status, smoke exposure, lack of breast-feeding, and contact with other children. None of these factors independently correlated with illness severity except for young age and prematurity.
What drug is used for RSV prophylaxis in high-risk infants and children?
A: Palivizumab (Synagis) is used as prophylaxis against RSV as a monthly injection in high-risk children. There is no RSV vaccine available.
---
New England Journal of Medicine - Vol. 360, No. 6, February 5, 2009
Hall CB et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med 2009 Feb 5; 360:588.
治骨鬆新藥 僅須1年打1針
年過五十歲的女性,約半數有骨質疏鬆症狀,但臨床調查發現,骨鬆患者服藥的持續性很不理想,不管是每日或每月劑型,超過五成患者會在治療一年左右即中斷用藥。醫界已就此現象研發出一年打一針的新藥,除了使用方便,實驗也證明該藥療效廣泛,可使髖骨骨折手術後的致死風險降低約三成。
新光醫院骨科主任魏志定昨說,此新藥名為「骨力強」,對患者最明顯好處為治療便利性高,只要躺或坐在病床上十五分鐘,以點滴注射,即可完成一年份用藥,但目前健保並未給付,每次自費價約兩萬五千元。
記者邱俊吉 /蘋果日報A11版
----------
Aclasta
----------
Generic Name: zoledronic acid
Brand names: Zometa, Zometa Concentrate, Aclasta, Reclast
Important information about Aclasta
通過FDA的新藥Aclasta,是目前最長效的治療骨質疏鬆症的藥,從FDA公佈的研究資料來看,新藥用於曾髖部骨折的病人身上,可降低死亡率28%,但副作用為心房顫動,發燒,肌肉,骨骼或關節疼痛,類似流感症狀以及頭痛等.
Do not receive Aclasta without telling your doctor if you have had an allergic reaction to zoledronic acid or similar medicine such as alendronate (Fosamax), etidronate (Didronel), ibandronate (Boniva), pamidronate (Aredia), risedronate (Actonel), or tiludronate (Skelid). Do not use Aclasta without telling your doctor if you are pregnant. It could cause harm to the unborn baby. Use an effective form of birth control, and tell your doctor if you become pregnant during treatment.
Your doctor may recommend you have a dental exam for preventive tooth and gum care before you start your treatment with Aclasta. This is especially important if you have cancer, if you are undergoing chemotherapy or using steroids, or if you have poor dental health.
Some people using medicines similar to Aclasta have developed bone loss in the jaw, also called osteonecrosis of the jaw. Symptoms of this condition may include jaw pain, swelling, numbness, loose teeth, gum infection, or slow healing after injury or surgery involving the gums. You may be more likely to develop osteonecrosis of the jaw if you have cancer or have been treated with chemotherapy, radiation, or steroids. Other conditions associated with osteonecrosis of the jaw include blood clotting disorders, anemia (low red blood cells), and pre-existing dental problems.
Avoid having any type of dental surgery while you are being treated with Aclasta. It may take longer than normal for you to recover.
---
http://www.drugs.com/aclasta.html
新光醫院骨科主任魏志定昨說,此新藥名為「骨力強」,對患者最明顯好處為治療便利性高,只要躺或坐在病床上十五分鐘,以點滴注射,即可完成一年份用藥,但目前健保並未給付,每次自費價約兩萬五千元。
記者邱俊吉 /蘋果日報A11版
----------
Aclasta
----------
Generic Name: zoledronic acid
Brand names: Zometa, Zometa Concentrate, Aclasta, Reclast
Important information about Aclasta
通過FDA的新藥Aclasta,是目前最長效的治療骨質疏鬆症的藥,從FDA公佈的研究資料來看,新藥用於曾髖部骨折的病人身上,可降低死亡率28%,但副作用為心房顫動,發燒,肌肉,骨骼或關節疼痛,類似流感症狀以及頭痛等.
Do not receive Aclasta without telling your doctor if you have had an allergic reaction to zoledronic acid or similar medicine such as alendronate (Fosamax), etidronate (Didronel), ibandronate (Boniva), pamidronate (Aredia), risedronate (Actonel), or tiludronate (Skelid). Do not use Aclasta without telling your doctor if you are pregnant. It could cause harm to the unborn baby. Use an effective form of birth control, and tell your doctor if you become pregnant during treatment.
Your doctor may recommend you have a dental exam for preventive tooth and gum care before you start your treatment with Aclasta. This is especially important if you have cancer, if you are undergoing chemotherapy or using steroids, or if you have poor dental health.
Some people using medicines similar to Aclasta have developed bone loss in the jaw, also called osteonecrosis of the jaw. Symptoms of this condition may include jaw pain, swelling, numbness, loose teeth, gum infection, or slow healing after injury or surgery involving the gums. You may be more likely to develop osteonecrosis of the jaw if you have cancer or have been treated with chemotherapy, radiation, or steroids. Other conditions associated with osteonecrosis of the jaw include blood clotting disorders, anemia (low red blood cells), and pre-existing dental problems.
Avoid having any type of dental surgery while you are being treated with Aclasta. It may take longer than normal for you to recover.
---
http://www.drugs.com/aclasta.html
2009年2月2日 星期一
Retroperitoneal pelvic packing
Direct retroperitoneal pelvic packing versus pelvic angiography: A comparison of two management protocols for haemodynamically unstable pelvic fractures
Objective
To evaluate the outcomes of haemodynamically unstable cases of pelvic ring injury treated with a protocol focused on either direct retroperitoneal pelvic packing or early pelvic angiography and embolisation.
Methods
A retrospective review of a prospectively collected database in an academic level I trauma centre, treating matched haemodynamically unstable cases of pelvic fracture with either pelvic packing (PACK group, n = 20) or early pelvic angiography (ANGIO group, n = 20). Physiological markers of haemorrhage, time to intervention, transfusion requirements, complications and early mortality were recorded.
Results
The PACK group underwent operative packing at a median of 45 min from admission; the median time to angiography in the ANGIO group was 130 min. The PACK group, but not the ANGIO group, demonstrated a significant decrease in blood transfusions over the next 24 h post intervention. In the ANGIO group, ten people required embolisation and six died, two from acute haemorrhage; in the PACK group, three people required embolisation; four died, none due to uncontrolled haemorrhage.
Conclusions
Pelvic packing is as effective as pelvic angiography for stabilising haemodynamically unstable casualties with pelvic fractures, decreases need for pelvic embolisation and post-procedure blood transfusions, and may reduce early mortality due to exsanguination from pelvic haemorrhage.
---
Injury Volume 40, Issue 1, January 2009, Pages 54-60
Objective
To evaluate the outcomes of haemodynamically unstable cases of pelvic ring injury treated with a protocol focused on either direct retroperitoneal pelvic packing or early pelvic angiography and embolisation.
Methods
A retrospective review of a prospectively collected database in an academic level I trauma centre, treating matched haemodynamically unstable cases of pelvic fracture with either pelvic packing (PACK group, n = 20) or early pelvic angiography (ANGIO group, n = 20). Physiological markers of haemorrhage, time to intervention, transfusion requirements, complications and early mortality were recorded.
Results
The PACK group underwent operative packing at a median of 45 min from admission; the median time to angiography in the ANGIO group was 130 min. The PACK group, but not the ANGIO group, demonstrated a significant decrease in blood transfusions over the next 24 h post intervention. In the ANGIO group, ten people required embolisation and six died, two from acute haemorrhage; in the PACK group, three people required embolisation; four died, none due to uncontrolled haemorrhage.
Conclusions
Pelvic packing is as effective as pelvic angiography for stabilising haemodynamically unstable casualties with pelvic fractures, decreases need for pelvic embolisation and post-procedure blood transfusions, and may reduce early mortality due to exsanguination from pelvic haemorrhage.
---
Injury Volume 40, Issue 1, January 2009, Pages 54-60
Pre-O2 should not > 4 min ??
Preoxygenation for Emergency Intubation: Longer Is Not Better
Preoxygenation beyond 4 minutes adds no benefit.
In critically ill patients, 3 to 5 minutes of preoxygenation with 100% oxygen through a resuscitator bag and mask is often recommended for patients who are spontaneously breathing and will undergo emergency intubation (JW Emerg Med Dec 1 1999). Researchers compared the effect of preoxygenation times of 4 versus 8 minutes on PaO2 in 34 patients in an intensive care unit who had preexisting arterial lines and required emergent or urgent intubation after noninvasive methods of hypoxia treatment failed. Arterial blood gas was measured during noninvasive management (baseline) and during preoxygenation at 4, 6, and 8 minutes. Investigators positioned patients to optimize airway patency and provided preoxygenation with 100% oxygen at 15 L/minute using a noncollapsing resuscitator bag and mask. Mean PaO2 was 62 mm Hg at baseline and increased to 84 mm Hg at 4 minutes. Further changes in mean PaO2 after 4 minutes were not significant.
Comment:
The real value of preoxygenation is not simply increasing PaO2 but rather prolonging the safe apnea time after administration of rapid sequence intubation drugs. This study is consistent with others that fail to show a benefit of prolonging preoxygenation beyond 3 or 4 minutes. Remember that a resuscitator bag used for preoxygenation must have a one-way exhalation valve to prevent entrainment of room air, which dramatically reduces the percentage of inspired oxygen (JW Emerg Med Nov 15 2000).
—
Tiffany M. Osborn, MD
Published in Journal Watch Emergency Medicine January 30, 2009
Citation(s): Mort TC et al. Extending the preoxygenation period from 4 to 8 mins in critically ill patients undergoing emergency intubation. Crit Care Med 2009 Jan; 37:68.
Preoxygenation beyond 4 minutes adds no benefit.
In critically ill patients, 3 to 5 minutes of preoxygenation with 100% oxygen through a resuscitator bag and mask is often recommended for patients who are spontaneously breathing and will undergo emergency intubation (JW Emerg Med Dec 1 1999). Researchers compared the effect of preoxygenation times of 4 versus 8 minutes on PaO2 in 34 patients in an intensive care unit who had preexisting arterial lines and required emergent or urgent intubation after noninvasive methods of hypoxia treatment failed. Arterial blood gas was measured during noninvasive management (baseline) and during preoxygenation at 4, 6, and 8 minutes. Investigators positioned patients to optimize airway patency and provided preoxygenation with 100% oxygen at 15 L/minute using a noncollapsing resuscitator bag and mask. Mean PaO2 was 62 mm Hg at baseline and increased to 84 mm Hg at 4 minutes. Further changes in mean PaO2 after 4 minutes were not significant.
Comment:
The real value of preoxygenation is not simply increasing PaO2 but rather prolonging the safe apnea time after administration of rapid sequence intubation drugs. This study is consistent with others that fail to show a benefit of prolonging preoxygenation beyond 3 or 4 minutes. Remember that a resuscitator bag used for preoxygenation must have a one-way exhalation valve to prevent entrainment of room air, which dramatically reduces the percentage of inspired oxygen (JW Emerg Med Nov 15 2000).
—
Tiffany M. Osborn, MD
Published in Journal Watch Emergency Medicine January 30, 2009
Citation(s): Mort TC et al. Extending the preoxygenation period from 4 to 8 mins in critically ill patients undergoing emergency intubation. Crit Care Med 2009 Jan; 37:68.
訂閱:
文章 (Atom)





